This includes the primary, secondary and tertiary (if any) insurance coverages of the patient. Insurance is of two types –
(1) Health plans and (2) Liability plans.
- Health plans are those coverages, which are subscribed to meet any health care costs/expenses.
- Liability plans are taken against any particular risk/accident. They are broadly classified as Auto accident plans and Workman’s compensation plans.
If the visit is for any accident (motor vehicle accident/auto accident or workman’s compensation) then the Date of accident/injury is included in the charge entry process.
Insurance details include:-
- Insurance name and address
- Insurance identification number
- Group name/Group number
- Validity of the policy
- Name of the insured (subscriber)
- Relationship of the insured to the patientDuring charge entry the primary insurance of the patient is billed according to the reason of visit by the patient.
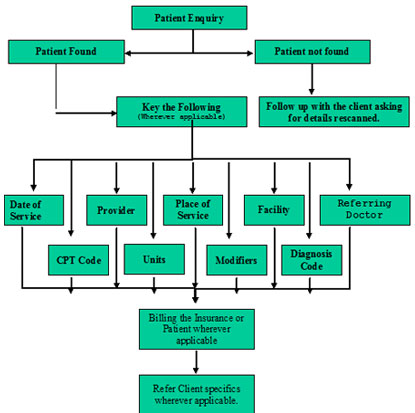
If all the demographic information is completed then the charge entry process can be continued with the following.
- Date of service:
The date of service is the date that describes the procedure/service performed in the charge sheet/charge ticket. According to the hospital(s), it is termed as Exam date or Service date or Ordering date on the reports.
- Billing provider:
The rendering physician who actually performs the services will be listed on the reports. The rendering physicians will be entered into the billing software according to the client specifications. The client specifications will have an associate of doctors who works in the hospital with their specialties.
- Place of service:
This is the place/facility where the services are actually performed by the rendering physicians. These are broadly classified as Outpatient Hospital services, Inpatient Hospital services and Emergency Hospital services. Every hospital will have a list of codes to specify the place of services where the services are performed.
- Admission date:
Date of hospital admission is necessary in case of all inpatient charges. The date of admission must be before the date of service.
- Referring physician:
This physician is the one who refers the patient(s) to the rendering physicians for the services performed.
The field on the charge sheet/ticket will have the following list as referring physicians according to client specifications.
They are:-
(a) Ordering physician
(b) Attending physician
(c) Admitting physician
(d) Family physician or Primary care physician (PCP)
(e) Copy for or Additional physician
- Referral #:
Referral number/Pre-certification number given on the reports will be entered along with the primary care physician name.
- Procedure code (CPT) and the number of units performed:
Current procedural terminology (CPT) is a standardized system of five-digit codes and descriptive terms used to report the medical services and procedures performed by physicians. These will be coded on the charge sheets or checked off on the charge tickets. If the procedure is performed more than once then it will also be specified as units on the charge sheets/charge tickets as per client specifications.
- Modifiers:
This is an extension of the procedure code, which further Explains treatment performed.Modifiers can indicate:
(1) A service or procedure has both a professional and a technical component.
(2) A service or procedure was performed by more than one physician
(3) Only part of a service was performed
(4) An adjunctive service was performed.
(5) A bilateral procedure was performed
(6) A service or procedure was provided more than once
(7) Unusual events occurred
- Diagnosis code:
The signs and symptoms for the visit are denoted as diagnosis codes. These are termed as International Classification of Diseases (ICD codes). The symptoms can be found in the History, Clinical data, Clinical history, Reason for exam, Reason for visit etc on the charge sheets/charge tickets according to the hospitals.
When all the above information is entered into the client billing software then the charge entry process is complete.